SUMMARY: As we close 2023 and look towards the new year of reporting with CMS, we walk through the requirements and changes CMS has made. This alert will serve as a guide on what you can expect and how you can best position yourself and your practice to comply with the Quality Payment Program. This update includes an overview of the MIPS program for 2024, including reporting requirements, measure updates and recommendations for anesthesia groups relative to overall participation.
At the end of the year, CMS provides the healthcare industry with the details of the upcoming reporting year with the Quality Payment Program (QPP); and, last Friday, they released the full list of registries that have been approved for reporting for 2024. Coronis Health has been approved for reporting as a Qualified Clinical Data Registry (QCDR) and a Qualified Registry (QR) for the ninth year, which not only allows us to support our clients in an engaged and supportive way but continues to allow us to be an active participant in the development and deployment of this program over the years. This release, along with the update to the 2024 Medicare Physician Fee Schedule (PFS) Final Rule, provides us with the full landscape of what CMS expects and how we are to comply with the QPP. This alert will walk through the requirements of 2024 reporting and be a resource to review if you have any questions about how you need to participate next year.
MIPS Category Review
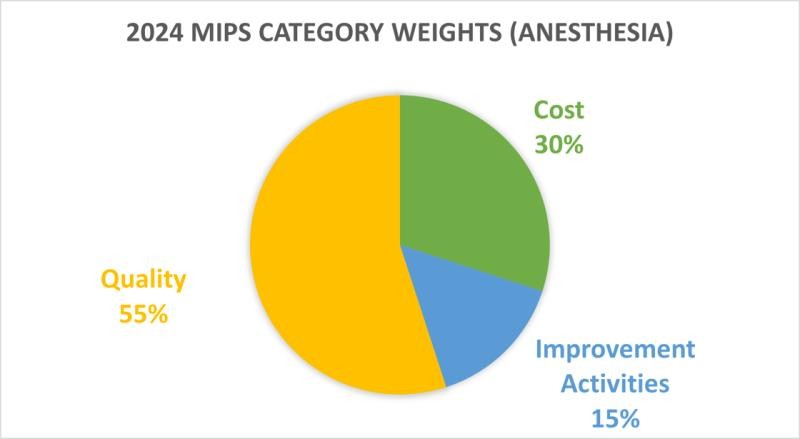
The QPP has two main payment tracks: the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APM). This update is going to primarily focus on the MIPS track, but we will make some references to the APM. If you have any questions about the APM reporting track, please reach out to your account executive so that we can check your eligibility. Under MIPS, there are four categories to consider, which are Quality, Cost, Improvement Activities and Promoting Interoperability. Some special considerations exist for anesthesia around these categories that we will walk through below. Your participation with MIPS should consider your needs with CMS compliance, strategic value of having this quality data tracked, and potential secondary benefits gained through your facility contracts or payer contracts. Based on your answers, you can review whether reporting through the traditional MIPS track or through a MIPS Value Pathway (MVP) is more advantageous and determine if you should report as an individual or as a group. This can get confusing quickly, but, hopefully, this review will clarify the program as it relates to anesthesia for 2024.
Previous years afforded anesthesia a bit of flexibility with reporting, and 2024 is thankfully no exception. This is primarily because CMS classifies the anesthesia specialty as “non-patient facing clinicians.” This status may be confusing given the nature of anesthesia care, but it is useful as it provides the specialty with options on how it chooses to participate with the QPP. One of the most important benefits is the automatic reweighting of the Promoting Interoperability (PI) MIPS category, which is the new version of the CMS 2012 Meaningful Use program. This is useful as it eliminates the requirement to comply with this category altogether and assigns the composite points that would be assigned to the Quality category. The Cost category is automatically calculated by the government, which leaves only the Quality and the Improvement Activities as the ones that anesthesia providers need to consider. Since CMS decided to keep the weighting of these categories stable for 2024, that means that the Quality category is worth 55 percent of your total score and Improvement Activities is worth 15 percent.
When your compliance in these categories is added together, a minimum of 75 points or more is required to avoid a penalty in 2024. The program isn’t all or nothing, however. 2024 reporting will result in a nine percent penalty assessed on your 2026 Medicare Part B payments if your total score is between 0 and 18.75 composite points. Anywhere from 18.76 to 74.99 composite points will assign a negative adjustment between nine percent and zero percent on a linear sliding scale. 75 composite points exactly will have a neutral adjustment, and anything above will have a sliding scale of a positive, but budget-neutral positive, adjustment. We don’t know exactly what this positive adjustment will be, but you can expect a maximum of around 3.5 percent of your 2026 Medicare Part B payments. This value may substantially increase as the COVID-19 hardship exemption ends, but we will update you if we see any major changes.
One other element of flexibility that anesthesia enjoys is that CMS includes a minimum threshold of collections from Medicare Part B payments. If a clinician collects less than $90,000 in traditional Medicare, they may be excluded from the program altogether. This doesn’t restrict your reporting if you want to participate and seek a bonus, but it may not obligate you if you have no interest. If you are curious about your status, you can search here with your NPI using the MIPS participation lookup tool. Coronis Health will review this on your behalf, as well, but feel free to check anytime.
Category Details – Quality & Improvement Activities
CMS updated the program with one big change. The data completeness requirement has increased to 75 percent for quality category reporting (up from 70 percent in 2023), meaning clinicians will need to report on 75 percent of each measure’s full year eligible population to be fully counted. There are a few more measures to choose from this year through the Coronis Health or the other anesthesia registries. The list of measures includes the following:
- #404: Anesthesiology Smoking Abstinence
- #424: Perioperative Temperature Management
- #430: Prevention of Post-Operative Nausea and Vomiting (PONY) - Combination Therapy
- #463: Prevention of Post-Operative Vomiting (POV)- Combination Therapy (Pediatrics)
- #477: Multimodal Pain Management (MIPS CQMs Specifications)
- #ABG41: Upper Extremity Nerve Blockade in Shoulder Surgery
- #ABG42: Known or Suspected Difficult Airway Mitigation Strategies
- #ABG43: Use of Capnography for non-Operating Room anesthesia Measure
- #AQI48: Patient-Reported Experience with Anesthesia
- #AQI56: Use of Neuraxial Techniques and/or Peripheral Nerve Blocks for Total Knee Arthroplasty (TKA)
- #AQI68: Obstructive Sleep Apnea: Mitigation Strategies
- #AQI69: Intraoperative Antibiotic Redosing
- #AQI71: Ambulatory Glucose Management
- #AQI72: Perioperative Anemia Management
- #AQI73: Prevention of Arterial Line-Related Bloodstream Infections
- #AQI67: Consultation for Frail Patients
- #ABG44: Low Flow Inhalational General Anesthesia
Under the traditional MIPS model, you would be required to report on at least six of the above measures. It will be important to choose the measures together with your team at Coronis Health as there are considerations around maximum scores achievable with the above measures through its historical benchmarks.
One thing to keep in mind is the final 2024 measures have not yet been published on the CMS website. These generally are viewable in the Resource Library, and we hope to see these posted by January 2, 2024. If there are any substantial changes to these measures, we will let you know; but, for now, review the above list, and you can select a minimum of six of them if participating in the traditional MIPS program.
Regarding Improvement Activities, there were some changes, but they don’t substantially affect anesthesia, with one exception. We will review this topic further in the next section, but CMS added an improvement activity for better support of the MIPS Value Pathways (MVPs). It is described as:
- IA_MVP: Practice-Wide Quality Improvement in MIPS Value Pathways
In essence, you can consider this improvement activity to double dip on MVP participation as it gives you an automatic credit for the category if you participate in an MVP. Given that support, there are a few considerations with MVPs for 2024.
MIPS Value Pathways
In 2023, CMS introduced the MVP reporting pathway as a method to simplify the entire process of reporting measures to CMS. In essence, the MVP provides a prescriptive list of options and a reduced burden of reporting to enable easier overall compliance with the QPP. This is a great way to comply; and, with Coronis Health as your partner, we will additionally work with you to maximize your bonuses. To do so, we will work on a combination of strategies to evaluate the best option with traditional MIPS, MVP, or, if you are a participant with ACO, through a reporting option called an APM (Advanced Alternate Payment Model). If you are participating in an ACO and have any questions about how the APM works, let your account executive know, and we can review your options.
The new year will include some potential changes with the MVP options for anesthesia. Currently, this is only published in the 2024 Medicare Physician Fee Schedule (PFS) Final Rule as a proposed change, but we will update you on the officially published MVP list when the QPP pages are updated. However, for this year, you can choose any four of the following measures if reporting through the Coronis Health QCDR:
- #404: Anesthesiology Smoking Abstinence
- #424: Perioperative Temperature Management
- #430: Prevention of Post-Operative Nausea and Vomiting (PONY) - Combination Therapy
- #463: Prevention of Post-Operative Vomiting (POV)- Combination Therapy (Pediatrics)
- #477: Multimodal Pain Management (MIPS CQMs Specifications)
- #487: Screening for Social Drivers of Health (NEW)
- AQI48: Patient-Reported Experience with Anesthesia
The MVP bundle additionally requires an Improvement Activity; but, as outlined above, the new measure (IA_MVP: Practice-Wide Quality Improvement in MIPS Value Pathways) allows providers to bypass this requirement by being able to double dip and not be overly concerned with the reporting of this category. However, if you are interested in reporting other improvement activities for an alternative reason, you can select two medium-weighted or one high-weighted improvement activity. The only catch to an MVP is that you must proactively register between April 1, 2024 and November 30, 2024, which Coronis Health can do on your behalf.
The measures to choose from are as follows:
Improvement Activities (2 Medium or 1 High)
- IA_BE_6: Regularly Assess Patient Experience of Care and Follow Up on Findings - High
- IA_BE_22: Improved practices that engage patients pre-visit - Medium
- IA_BMH_2: Tobacco use - Medium
- IA_CC_2: Implementation of improvements that contribute to more timely communication of test results - Medium
- IA_CC_15: PSH Care Coordination - High
- IA_CC_19: Tracking of clinician's relationship to and responsibility for a patient by reporting MACRA patient relationship codes - High
- IA_EPA_1: Provide 24/7 Access to MIPS Eligible Clinicians or Groups Who Have Real-Time Access to Patient's Medical Records – High
- IA_MVP: Practice-Wide Quality Improvement in MIPS Value Pathways – High
- IA_PCMH: Electronic Submission of Patient Centered Medical Home accreditation - High
- IA_PSPA_1: Participation in an AHRQ-listed patient safety organization – Medium
- IA_PSPA_7: Use of QCDR data for ongoing practice assessment and improvements - Medium
- IA_PSPA_16: Use of decision support and standardized treatment protocols - Medium
The MVP option may be the easiest way to comply with the QPP requirements for 2024, but we can work with you to be strategic about your measure selections to achieve the maximum composite points possible. Feel free to review the details of the MVP at the CMS website.
More information will be coming from us about the registration process but consider the MVP as your easiest avenue to meet overall QPP compliance for 2024. Until then, if you have questions about this topic, please contact your account executive or you can reach out to us at info@coronishealth.com.