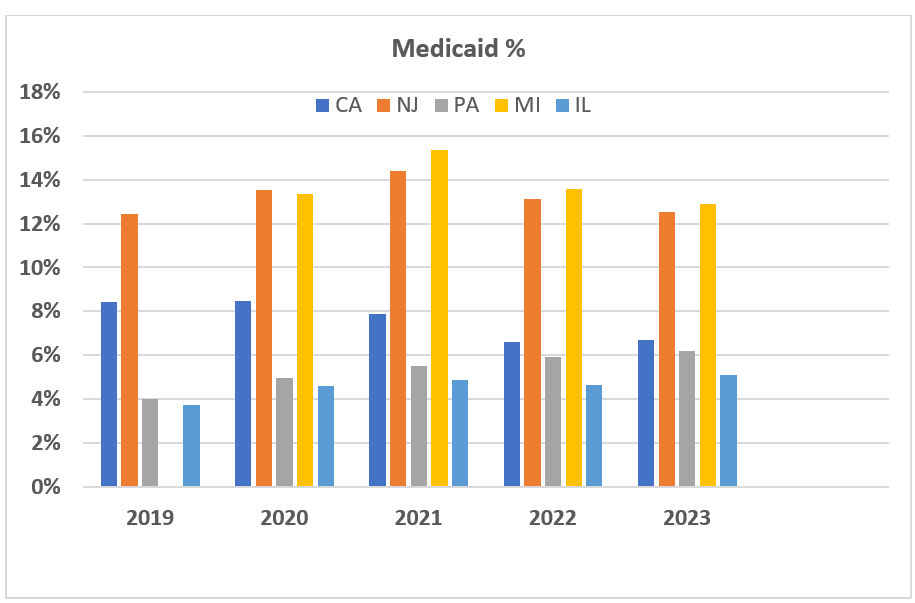
The impact of Medicaid varies considerably based on the location of the practice. The chart below represents the impact of Medicaid for five practices across the country over a period of five years. The increases in 2020 and 2021 were the result of Covid.
While Medicare guidelines are standardized across the entire country, each state has its own Medicaid plan; and, in most states, the Medicaid rate is lower than the Medicare rate, which is a result of state budgetary considerations. The Medicaid rate in New York, for example, is a paltry $10.00 per ASA unit, while Arizona pays $22.57 per unit. Alaska has the highest rate at $42.90 per unit. It should also be noted that, while Medicare rates are adjusted and updated each year, Medicaid rates rarely change.
Medicare includes both traditional Medicare plans and managed Medicare plans. While the payment rates may be different, the basic rules are usually the same. This is not the case for Medicaid where many states have implemented some dramatic alternatives to help keep the overall cost of the Medicaid plan down. The most notable of these is the Arizona plan called AHCCCS, which stands for Arizona Health Care Cost Containment System. The challenge with these managed care plans is that they often have unique eligibility rules and payment guidelines. Los Angeles probably has the greatest variety of such plans, which makes processing claims a real challenge.
The fundamental reality is that getting paid for Medicaid is all about eligibility. Coverage is always tied to specifical financial criteria and is often for a limited period. Many patients may believe they have Medicaid, in which case they will be listed as Medicaid eligible. Actual Medicaid coverage may or may not be available.
What should every provider know about Medicaid coverage?
- It is essential that one know the state rules; and, if the practice treats patients from multiple states, the rules must be known for each state.
- Anesthesia time is generally reported in 15-minute units, except in Illinois.
- Obstetric anesthesia claims are often subject to different rules. For example, surgical claims are paid at one rate, while obstetric claims are paid at a higher rate.
- Medically directed cases may also involve different rules and rates. In California, the CRNA payment rate is only a percentage of the surgical payment rate.
- Flat fee services, such as those for invasive monitoring and nerve blocks, are paid from a surgical fee schedule, but in some cases may be considered inclusive with the anesthesia service.
Many providers tend to lump self-pay and Medicaid together because the net yield is so low. It is often said that any money collected for Medicaid claims is “found money” because the rules are in some cases so arcane. Some payment is better than no payment. Sometimes, the cost of collecting a Medicaid claim is greater than the amount collected. It is important to keep this in perspective. Despite the net yield, though, Medicaid collections are still an important piece of the revenue puzzle. If you have questions about this topic, please contact your account executive.
