What is the Merit-based Incentive Payment System?
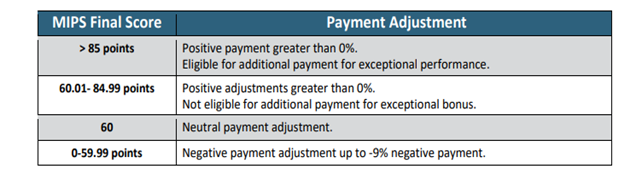
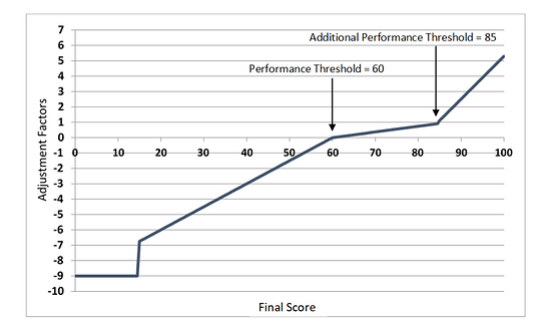
The performance threshold for 2021 is 60 points, which means:
- A MIPS score below 60 points will result in a negative payment adjustment
- A MIPS score above 60 points will result in a positive payment adjustment
2021 Final Performance Threshold & Payment Adjustment
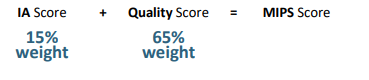
How is MIPS Scored?
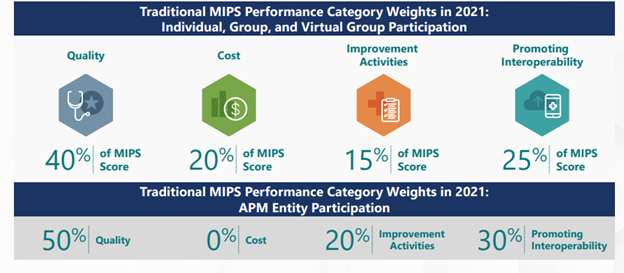
The MIPS performance categories have different “weights,” and the scores from each of the categories are added together to give you a MIPS Final Score.
Step 1: Check Your Current Eligibility
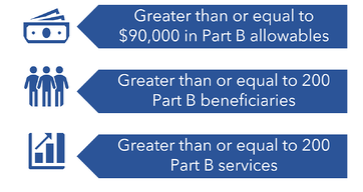
MIPS payment adjustments are only applicable to clinicians deemed “MIPS eligible.”
The low volume threshold includes 3 aspects of covered professional services:
Step 2: Select and Perform Your Measures and Activities
Quality Category 40% of MIPS Score
Sixty (60) performance points are needed to earn full credit for the Quality category. Most clinicians must select 6 measures, including 1 outcome/high priority measure, by exploring these measures and collecting data for each measure for the 12-month performance period (January 1- December 31, 2021).
NOTE: Clinicians in SMALL practices automatically receive six points in their quality category if at least one quality measure is reported. This is called the small practice bonus.
Improvement Activity Category 15% of MIPS Score
Easiest category and points to earn! Forty (40) performance points are needed to earn full credit for the improvement activity (IA) category. Practices receive full credit for the IA category when they complete:
- 2 high-weighted activities,
- 1 high-weighted activity and 2 medium-weighted activities, or
- 4 medium-weighted activities
How Should You Submit Data? There are 3 submission types you can use for improvement activities, depending on which submitter type you are. The submission types are:
Promoting Interoperability Category 25% of MIPS Score
One hundred (100) performance points are needed to earn full credit for the promoting interoperability (PI) category. All required PI measures must be reported or excluded. When a measure is excluded, the points are reallocated to a different, assigned PI measure. You must submit collected data for certain measures from each of the 4 objectives measures (unless an exclusion is claimed) for 90 continuous days (or more) during 2021. Additional requirements for this category include use of a 2015 edition certified electronic health record (EHR) and you must provide your EHR’s CMS Identification code from the Certified Health Product List and submit a “yes” to:
- The Prevention of Information Blocking Attestation,
- The ONC Direct Review Attestation, and
- The security risk analysis measure.
Additional help on this category: PI Requirements, Hardship Exceptions, How to Submit Data Links
Cost Category 20% of MIPS Score
You do not have to submit ANY data for this performance category!
For performance year 2021, CMS will use cost measures that assess: the overall cost of care provided to Medicare patients with a focus on the primary care they received, the cost of services provided to Medicare patients related to a hospital stay, and costs for items and services provided.
CMS determines measure achievement points by comparing performance on a measure to a benchmark. CMS calculates cost measure benchmarks using performance data from the performance period, rather than historical benchmarks.
Additional Help on this Category: Cost Quick Start Guide
Step 3: Understand How COVID-19 Relief Efforts Affect 2021 MIPS Payment Adjustments
The COVID-19 pandemic has impacted all clinicians across the United States and territories. However, CMS recognizes that not all practices have been impacted by COVID-19 to the same extent. For PY2021, CMS will continue to use the extreme and uncontrollable circumstances policy to allow clinicians, groups, virtual groups, and APM Entities to apply requests for reweighting of performance categories due to the current COVID-19 public health emergency.
There are two exception applications available to clinicians in PY2021:
- The Extreme and Uncontrollable Circumstances Exception application allows you to request reweighting for any or all performance categories if you encounter an extreme and uncontrollable circumstance or public health emergency, such as COVID-19, that is outside of your control.
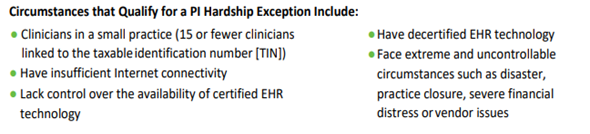
- The MIPS Promoting Interoperability Performance Category Hardship Exception application allows you to request reweighting specifically for the Promoting Interoperability performance category if you qualify for one of the reasons identified below. This application is available for the following specified reasons:
- You’re a small practice
- You have decertified EHR technology
- You have insufficient Internet connectivity
- You face extreme and uncontrollable circumstances such as disaster, practice closure, severe financial distress or vendor issues
- You lack control over the availability of CEHRT
- You’re a small practice
- You have decertified EHR technology
- You have insufficient Internet connectivity
- You face extreme and uncontrollable circumstances such as disaster, practice closure, severe financial distress or vendor issues
- You lack control over the availability of CEHRT
- You’re a small practice
- You have decertified EHR technology
- You have insufficient Internet connectivity
- You face extreme and uncontrollable circumstances such as disaster, practice closure, severe financial distress or vendor issues
- You lack control over the availability of CEHRT
What Happens If Your Application is Approved?
If your application is approved, you don’t have to report for the requested MIPS performance category or categories, and those categories will be reweighted.
- Application deadlines are December 31, 2021 at 8PM ET.
Step 4: Report Categories Based on YOUR Circumstances:
The MIPS 2021 final rule is for calculating the MIPS payment adjustment for your composite score. Remember you only need 60 points to avoid the negative payment adjustment of -9% in 2023:
Scenarios to Avoid the Adjustment include:
- Scenario 1: You do not have an EHR. If you do not have a 2015 edition certified EHR, you CAN still participate in MIPS. You can report the Quality and IA categories and apply for a PI Hardship Exception, because you are a SMALL practice.
- Scenario 2: You have an EHR. If you have a 2015 edition certified EHR, you can submit data in the Quality, IA and PI categories or just the Quality and IA categories, if you submit a PI Hardship Exception application and it is approved.
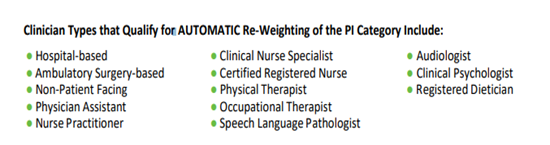
- Scenario 3: The PI category is automatically reweighted. If you are a clinician type listed below, CMS automatically re-assigns the PI category points to the Quality category. As a result, you only need to report the Quality and IA categories to earn 60 points.
- Scenario 4: The PI category is reweighted due to an approved PI Hardship Exception Application. If you are a clinician or group and one of the following circumstances applies, you can submit a PI Hardship Exception application. If the application is approved, you only need to report the Quality and IA categories.
Step 5: Submit Your Data
- Submit data yourself or with the help of a third-party intermediary, such as a Qualified Registry or Qualified Clinical Data Registry (QCDR), between January 3 and March 31, 2022.
- Visit the Quality Payment Program Resource Library to review the lists of CMS-approved Registries Qualified Registries and QCDRs.
Step 6: Review your Feedback
Review your preliminary feedback, available once data is submitted. Review your final performance feedback and payment adjustment information in July 2022.
When you successfully submit a valid quality data code (QDC), the RA/EOB will list the RARC code N620 which means that the QDC got to our NCH database.
- If you bill with $0.00 charge on a QDC line item, you’ll get an N620 code on the EOB. N620 says: Alert: This procedure code is for quality reporting/informational purposes only.
Questions:
- Please visit the Quality Payment Program web portal - https://qpp.cms.gov/
- Contact CMS – call the Quality Payment Program Service Center at 1-866-288-8292
