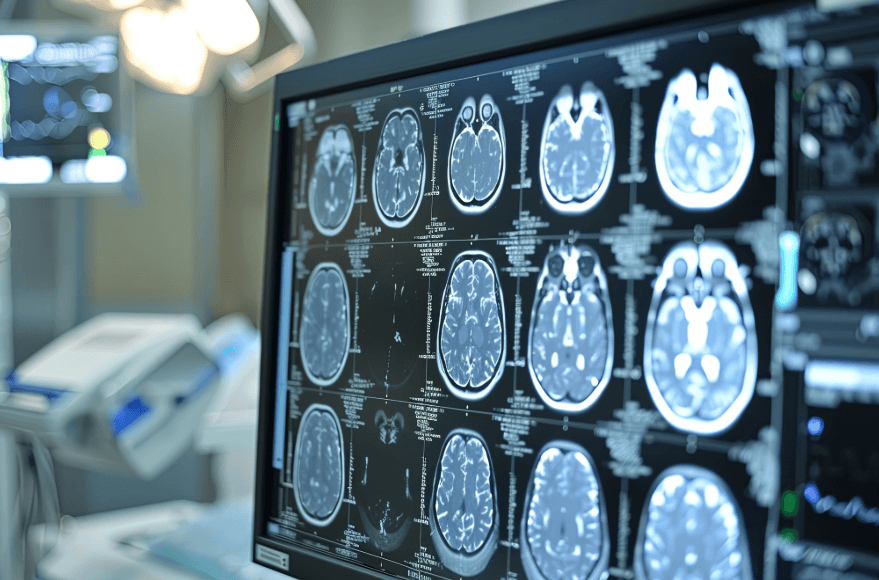
Although this is primarily a problem for older patients, no patient is immune to the potential for strokes. Many factors may increase the risk. These include obesity, lack of exercise, smoking and genetics. There are various treatment options that are possible; but clearly, timing is critical. Since a stroke causes a lack of adequate blood flow to the brain, the longer it takes to initiate effective treatment, the more severe the damage will be, and the longer recovery will take.
As the number of stroke patients increases, many hospitals are developing more formal stroke programs. Most are starting to rely more extensively on appropriate anesthesia care to support the endoscopic procedures provided by the interventional radiologists. Clearly, the primary role of the anesthesia provider is to ensure oxygenation and blood pressure management. As the parameters of treatment continue to be refined, the role of anesthesia becomes more significant and important. This is causing many anesthesia practices to evaluate the requirements and revenue potential of a dedicated service.
Documentation Requirements
A review of stroke cases from a wide variety of Coronis clients reveals a variety of treatment modalities. Anesthesia for acute stroke procedures are typically performed with either a general or MAC anesthesia type.
From a billing perspective, documentation requirements on the anesthesia record are the same as with any other anesthesia procedure. The appropriate ASA code depends on the particular circumstances of the diagnostic/therapeutic stroke-related procedure. Several codes may be in play. One such code is 01922, anesthesia for non-invasive imaging, with a base value of seven units, when a diagnostic CT of the head/brain is performed. As is typical for surgical cases, the anesthesia time reflects the continuum of care during which there is a relationship of dependence between patient and provider. Anesthesia times can vary from 45 minutes to three hours (three time units to 12 time units). Obviously, payment is a function of the patient’s insurance, and the majority of stroke patients are covered by Medicare, which has a significantly discounted rate.
Planning for the Future
From a strategic perspective, anesthesia practices should always be focused on anticipating the needs of the facility. Given an aging population and the critical role anesthesia can play in the management of stroke patients, this is an area all practices should be focused on and assessing.